- What is this Coxiella pathogen?
Coxiella burnetii is a Gram-negative bacterium that infects animals and humans causing the Q fever (query fever). This is a strictly intracellular pathogen that encodes several basic proteins and buffers to acidic pH the environment of the phagolysosome-like vacuole. The genome of this bacterium includes 4 Na+ exchangers and transporters for molecules that protect the cells from osmotic and oxidative stress.
The Coxiella’s life cycle contains 2 forms of development – large-cell (LCV) or the active replicating form found during the log phase and small-cell variant (SCV) that are typical for the stationary phase. SCVs show a significant resistance to various stressful factors of the environment – mechanical, heat, chemical, changes in the osmotic levels. Many reports describe the survival of the Coxiella cells on wool at room temperature for up to 1 year, in milk for more than 3 years, and in fresh meat for 4 weeks. The Coxiella burnetii is characterized as highly virulent and can be transmitted by aerosols. Due to this, U.S. Centers for Disease Control and Prevention categorized this pathogenic agent as Class B bacteria. The infection is not observed with high death rate, but it can lead to persistent disease and cause disability and serious consequences for the human population health status.

2. How to recognize the Q-fever infection?
The main mammalian sources of Coxiella burnetii are ruminants – goats, sheep, cattle. The disease has been reported in almost all regions, except in New Zealand. The epidemiological levels of Q fever highly vary for the different countries and it depends on the geographic area and endemic profile. Scientists focused on the disease in 1999. Then, in The United States, the spread of the disease had led to 250% more cases of infected people in the period of 2000-2004. In Martigues (France), every 34 citizens from 100 000 were diagnosed with Q fever. More than 4000 cases were reported in The Netherlands between 2007 and 2010. An epidemic situation occurred in French Guiana due to the high virulence and stability of Coxiella burnetii cells. Normally, Q fever is not an acute disease and it is observed with flu-like symptoms. Most people infected with Coxiella burnetii have no symptoms at all.
However, there are cases of patients who get ill years after the infection. This is a result of an acute Q fever that can damage lungs, heart, liver. Q fever can be transmitted from animals to humans through urine, feces, milk and via inhalation of Coxiella burnetii-contaminated barnyard dust particles. The risk from infection is highest for groups like farmers, vets and researchers in field of veterinarian medicine and animal care. Q fever is cured quickly with antibiotic therapy but sometimes the treatment could take up to 1,5 years.
The symptoms occur between 3 and 30 days after exposure to Coxiella burnetii and may include high fever (more than 39 degrees Celsius), vomiting, cough, nausea, chills, fatigue, diarrhea, sensitivity to light.
Along with the location in a farm or near to farms or farming facilities, another risky factor is the time of the year – highest numbers of acute Q fever infected people are reported in April and May in The United States. Some reports show that the men are more likely to develop acute Q fever symptoms than women.
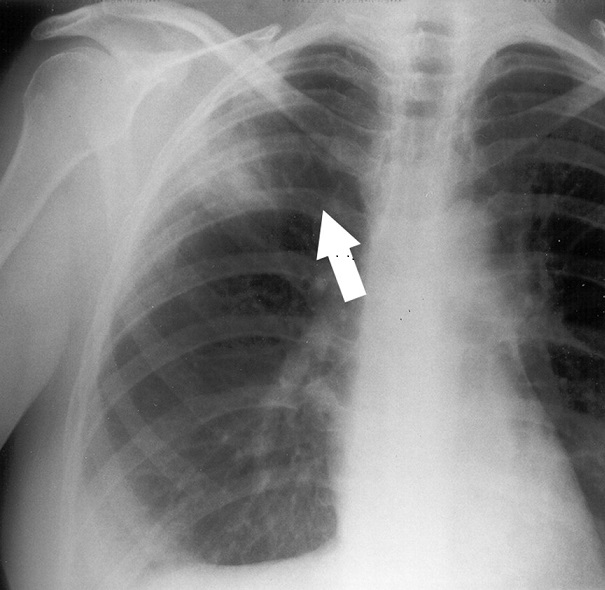
The risk of developing the acute form of Q fever (sometimes with lethal end) is higher for people with heart valve disease, weakened immune system, damaged kidney function, complications. The deadliest complication as a result of a Q fever recurrence is endocarditis. Q fever infected people can also develop pneumonia and acute respiratory distress. Pregnant women with chronic Q fever could have problems like low birth weight, premature birth or miscarriage. Other complications are observed with livers – people could have hepatitis due to Q fever infection, and brain meningitis – an inflammation of the membrane surrounding the brain and spinal cord.
The prevention from Q fever includes vaccination for people who live in high-risk locations. The vaccine has been developed in Australia, 1989. The infection with Coxiella burnetii can be avoided with a consummation of pasteurized milk and pasteurized milk products only.
3. Which are the techniques used for diagnosis of Q fever?
The reference technique for detection of Coxiella burnetii is Indirect immunofluorescence assay (IFA) but other serology methods as complement fixation test (CFT) and ELISA are also used. Only kits and reagents for these assays are available on the market. ELISA has several advantages because it is easy to perform, the assay can be automated, and it is mainly used for diagnosis of acute and chronic Q fever. The most sensitive technique was IFA for detection IgM antibodies at an early phase of infection and after 12 months of follow-up. The sensitivity of CFT is reported as too low to be used for diagnosis and follow-up of C. burnetii persistent infection.
Several PCR-based analyses have been developed for the detection of Coxiella burnetii in clinical samples. The first standard PCR systems amplified plasmid sequences, the 16S-23S RNA, the superoxide dismutase gene, the com1 gene or the IS1111 repetitive elements in human or animal samples. Real-time PCR/qPCR is reported as faster and more sensitive PCR technique that provides information for the bacterium quantity in the tested clinical samples. Due to this, the qPCR assay is the most frequently used for detection of Coxiella burnetii these days. It targets IS1111 and can detect the bacterium within 2 weeks after exposure. Real-time PCR is also used for detection of persisting Coxiella burnetii infection in patients’ blood samples. The isolation and culturing of Coxiella burnetii is still used in many clinics and it can be achieved through the shell vial technique.
A new and interesting tool for detection of this pathogen is Immuno-PCR technique. It combines the PCR amplification with ELISA’s specificity and versatility which results in higher sensitivity. Many studies report that Immuno-PCR has significantly better sensitivity than ELISA and IFA in serum samples collected during the first 2 weeks after the symptoms’ development.
Nowadays, the scientists are mainly focused on understanding the factors that could decrease the virulence of Coxiella burnetii. This will allow the development of effective strategies for treatment and prevention of Q fever and avoid the risk from complications such as endocarditis, hepatitis and pneumonia in patients from all over the world.